How Veins Work and When They Don't
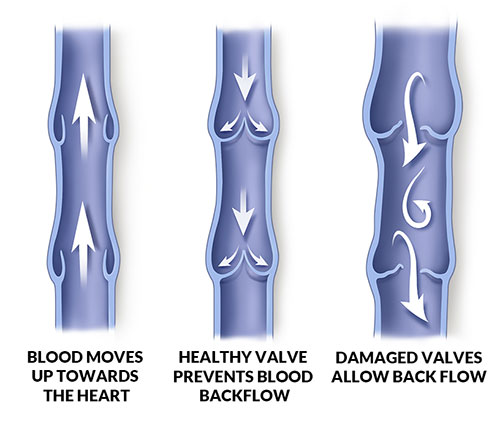
Veins are the blood vessels that return blood to the heart from the body. To overcome the force of gravity, the veins have one-way valves that open to allow blood flow to the heart and close to prevent “reflux” of blood back to the body. When these valves fail to function, or if the vein is damaged so the valves do not completely close, blood can begin to pool in the veins and cause a variety of complications.
Symptoms–From Spider/Varicose Veins to Complex Vein Diseases
At the Vein Center of Austin Heart, our cardiologists know how vein problems and diseases affect the entire cardiovascular system. Most vein disease can be seen by examining the size and color of the vein at the skin surface. In other cases, the diseased vein may be deeper in the body and not visible through the skin. Symptoms of vein disease include:
- Spider or “broken” veins
- Bulging varicose veins
- Leg or ankle swelling
- Painful, aching, cramping legs
- Leg heaviness and fatigue
- Dry, flaky skin
- Discolored skin (brown, purple, red)
- Skin breakdown or ulcers
Types of Vein Disease
Vein disease is a ‘progressive’ disorder because, if left untreated, it is more likely to turn into more serious problems. So when a patient comes in, whether with spider veins or serious symptoms, our cardiologist will do a thorough evaluation. Varicose veins and spider veins usually can be treated in the office with little or no pain and a quick recovery. More serious problems in the veins, such as blood clots, can put your life at risk. It’s always a good idea to check with your doctor to identify the problem and learn as much as you can about your options for treatment.
Chronic Venous Insufficiency (CVI) or Venous Reflux Disease
CVI is damage or weakness in the vein wall or vein valve that allows blood to flow back into the vein (venous reflux). The backflow of blood accumulates in the veins and causes inflammation (phlebitis) and more clotting. Clotting can block or slow blood flow through the vein raising blood pressure and possibly causing more damage. When pressure in the veins continues for a long time, it can break down healthy tissue, which causes ulcers or sores.
Varicose and spider veins are caused by venous reflux.

Spider Veins
Spider veins are small, thread-like colored veins that are most often seen on the surface of the skin. While many people seek treatment for spider veins for cosmetic reasons, spider veins also can result in substantial discomfort that require additional therapy.
Varicose Veins
Large, “rope-like” veins which are often ¼” or larger in diameter, varicose veins generally grow in size over time and can result in substantial pain and complications if not treated. Varicose veins generally worsen over time. Initially, slight pain and restlessness in the diseased leg will be felt. If untreated, this pain will increase and result in limitations in walking and cramps during sleeping. Eventually, varicose veins can lead to open sores on the foot, blood clots and tissue loss.
Phlebitis
Swelling in the deep or superficial veins is called phlebitis.
Other Serious Vein Diseases
Thrombosis
A blood clot in the vein. Blood clots can block blood flow or break free and travel through the blood stream to the heart and lungs (pulmonary embolism).
Thrombophlebitis
Swelling caused by a blood clot in the vein. It can occur in the superficial or deep veins.
Deep Vein Thrombosis (DVT)
With DVT, blood clots form in the large veins deep within the legs, pelvis, and sometimes in the arms. DVT strikes about 1 in 20 people over the course of a lifetime. DVT can also lead to complications in the legs referred to as chronic venous insufficiency. This condition is characterized by pooling of blood, chronic leg swelling, increased pressure, increased pigmentation or discoloration of the skin, and leg ulcers known as venous stasis ulcer.
Even though DVT itself is not life-threatening, the blood clot has the potential to break free and travel through the bloodstream, where it can become lodged in the blood vessels of the lung (known as a pulmonary embolism). This can be a life-threatening condition.
Pulmonary Embolism (PE)
When a blood clot breaks free from a deep vein and makes its way into an artery in the lung, it is called a pulmonary embolism (PE). PE is a life-threatening condition that can cause heart failure. It is important to call 911 if you have trouble breathing or if you are coughing up blood.
Post-Thrombotic Syndrome
(Also known as postphlebitic syndrome and venous stress disorder) In this condition, the symptoms of pain, heaviness in the leg or foot, cramps, itching, tingling, bluish or brownish flaky skin, sores, and varicose veins caused by DVT continue after treatment, either because the blood clot is still there or the blood clot caused other damage to the vein.
May Thurner Syndrome (MTS)
Most people do not know they have MTS, but it can be identified when they present with a deep vein thrombosis (DVT). Also known as Iliac Vein Compression Syndrome, it is an asymmetrical swelling of the legs – the left leg swells but the right leg does not. In its milder forms, the leg may not even swell. One side may simply have more severe vein disease than the other. MTS is a common condition.
Paget–Schroetter Disease
This disease is a form of upper extremity deep vein thrombosis (DVT), a medical condition in which blood clots form in the deep veins of the arms.
Diagnosing Vein Disease

Ultrasound Tests
These are painless tests that use sound waves to create images that help diagnose vein problems. We use both a hand-held Doppler ultrasound test to listen to blood flow and a duplex ultrasound to look at the structure of your veins and uncover any problem affecting the flow of blood through your veins.
